CONTACT
Thanks for your interest in Science Creates. So we can get you to the correct team member, please tell us what you are looking for?
Discover more about the scientists working to develop vaccines, treatments and a better understanding of the virus
There’s a lot that we still don’t know about SARS-CoV-2. Researchers in Bristol responded quickly at the start of the pandemic, pooling their collective knowledge, research and equipment to learn more about the virus and look at ways to develop new vaccines and treatments for it. They have made some incredible advances. We spoke to some of the key players about what’s been happening behind the lab doors and in hastily-prepared home offices across Bristol.
Bristol UNCOVER
In March, concerned researchers in Bristol came together to form the Bristol University COVID-19 Emergency Research Group (UNCOVER). Initially they held virtual 9am meetings seven days a week to answer each other’s questions and identify opportunities to work together. The group is still growing and evolving, and it isn’t exclusive: virologists, immunologists, clinicians, aerosol scientists, mathematicians, and more disciplines are represented. UNCOVER is being coordinated by Professor Adam Finn, Director of the Bristol Children’s Vaccine Centre, who has worked on vaccine trials for nearly 30 years. He discussed Bristol’s response to COVID-19 with us over the phone:
‘I’ve always known that the University of Bristol is a friendly environment: we prefer cooperation over competition, but the response to COVID-19 has surprised me. I thought I’d met everyone I’d want to work with, but the crisis has flushed us all out and brought us together – I’ve even discovered new collaborators in my own building! I’m proud of how many interdisciplinary projects we’ve got going, with goals that individual researchers couldn’t reach alone. It’s only by working together that we’ll be able to find solutions.
‘Bristol is just one part of the team effort across the world, but we are well-placed to contribute. Andrew Davidson and David Matthews were some of the only people in the world studying coronaviruses before the pandemic, and their experience is critical. The University of Bristol has a powerful synthetic biology capacity, which has allowed us to produce the biological materials required for coronavirus studies around the country. We’re strong in both clinical and lab research, and the fluent interface between the two has accelerated our understanding of the virus.
‘Bristol also has a wealth of experience in running vaccine trials, and we’re one of five centres involved in testing the Oxford vaccine candidate on healthy volunteers. If you’d told me a year ago that we’d be able to test a vaccine candidate in 9,000 people just six months after discovering a virus, I wouldn’t have believed you but we’re already beginning to understand the body’s response to this promising treatment: keep an eye out for details in The Lancet soon.
‘I’m an optimist. Our species has been so successful because we’re adaptable and resourceful. That we’ve managed to control the spread of SARS-CoV-2 is a testament to those qualities, and now the best minds on the planet are focused on beating this pandemic. But we can’t be complacent. Experts were warning for decades that a crisis like this was coming, but we weren’t ready, and precious time was lost. We can’t be caught on our heels next time.’

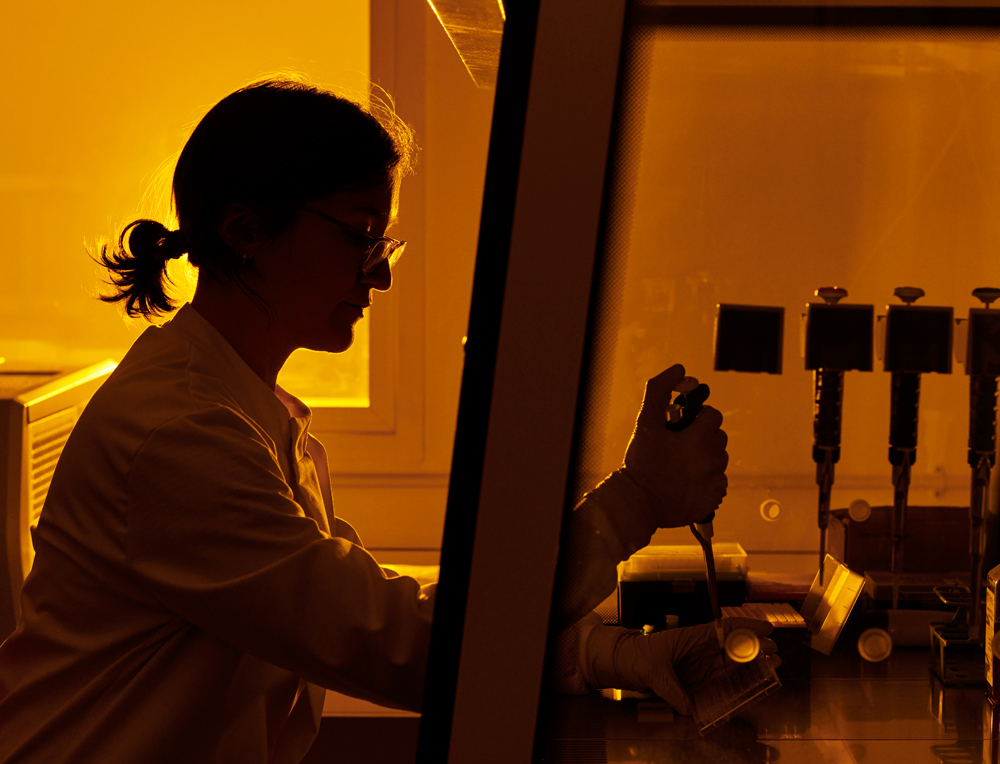
Cryo EM
SARS-CoV-2 is just one member of a family of coronaviruses, most of which are relatively harmless. Several features of SARS-CoV-2 have combined to make it particularly deadly:
• High infectivity – it easily spreads between people and establishes new infections
• Severe pathology – it produces a disease with serious symptoms, a high mortality rate, and long-term health effects
• Broad tissue tropism – it can infect many different types of cells and tissues in the body
How does the virus do it? A key idea in biology is that the shape of a molecule (its structure) controls what it can do (its function). Scientists especially want to know more about the SARSCoV-2 spike protein, which allows the virus to invade human cells, so researchers at the University of Bristol decided to study its structure using cryogenic electron microscopy (cryo-EM).
Cryo-EM is a powerful technique that won the Nobel prize in chemistry in 2017. A very pure solution of a particular protein is transferred to a metal mesh and rapidly frozen to -190 oC. A beam of electrons is then fired at the mesh, projecting an image of the proteins onto an electronic detector. Because the wavelength of electrons is much shorter than that of visible light, it produces much higher resolution images than a light microscope, revealing the fine details of molecules.
Professor Christiane Berger-Schaffitzel is the academic lead for the state-of-the-art £3.7 million GW4 cryo-EM facility based at the University of Bristol. As part of UNCOVER, her group produced a new structure of the SARSCoV-2 spike protein. Some of the greatest advances in science owe a lot to serendipity: microwaves, penicillin, and LSD to name a few. It just so happens that to produce the spike protein [for structural studies] Professor BergerSchaffitzel uses a media, a kind of salty soup that cells like to grow in, that contains cod liver oil. Cod liver oil contains lots of different fats, but out of this mixture, the spike protein specifically binds linoleic acid. In fact, it manages to hang on to this fatty acid throughout the harsh cryo-EM sample preparation process, which suggests that this interaction is important.
None of the previously published structures of SARS-CoV-2 include linoleic acid, but when the spike protein binds this molecule, its shape changes in significant ways that may affect how the virus binds and infects cells. Disrupting the interaction of the spike protein and linoleic acid could be a good target for drugs that fight SARS-CoV-2.
Professor Berger-Schaffitzel explains: ‘Once inside human cells, coronaviruses change the ways that their hosts use fatty acids. This can interfere with communication between cells, leading to inflammation and damage to the body, especially to the lungs. There’s evidence that linoleic acid is at the ‘crossroads’ of the different biochemical pathways that coronaviruses alter, so the ability of SARS-CoV-2 to tightly bind this molecule could be a major reason that this virus is so much more dangerous than its relatives.

Imophoron
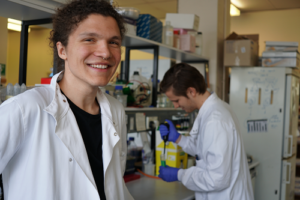
Imophoron is a start-up based at the Science Creates St Philips incubator in Bristol, founded by Frederic Garzoni [pictured above] and Prof Imre Berger using technology developed at an institution in France.
The best way to beat viruses is by vaccination. The World Health Organisation estimates that vaccination saves 2-3 million lives every year. Vaccines rally the body’s immune system to prevent viral infections. Importantly, being vaccinated doesn’t just protect you – it protects your community. If you can’t be infected by a virus, you also can’t pass it on, which protects the vulnerable people around you from infection. As more people in a population are vaccinated and become immune, the spread of a virus is slowed, and eventually the disease can be eradicated.
As of the 12th of November, the World Health Organisation reports that 48 COVID-19 vaccine candidates are in clinical trials, and 164 are at preclinical stages. Excitingly, one of these vaccines is being developed by Imophoron at a Science Creates incubator. Imophoron was founded by Frédéric Garzoni and Professor Imre Berger in 2017 to develop the ADDomer©, a novel vaccine platform for emerging infectious diseases and unmet medical needs. The ADDomer is based on a single component of the human adenovirus that spontaneously forms a superparticle.
During an infection, the immune system recognises antigens on the invading pathogen and produces antibodies to specifically bind them, neutralising the pathogen. But this process is slow, and some diseases can kill before the immune system is up to speed. That’s where vaccination comes in; we expose the immune system to antigens in a controlled and safe way so that it makes effective antibodies that will protect against the real disease in the future.
There are many types of vaccine. Some involve weakening a virus so that it will only cause a mild infection, although there’s a risk that the virus may ‘reactivate’ and cause serious disease. Others present just the viral antigens to the immune system but require additives called ‘adjuvants’ to activate the immune system; some people refuse vaccination because of concerns about adjuvants.
Imophoron’s technology is totally synthetic, so it cannot become infectious, and it doesn’t require adjuvants. The ADDomer can be easily and rationally engineered to present different viral antigens on its surface, allowing Imophoron to quickly react to new diseases. Imophoron’s CEO Frédéric Garzoni explains: ‘As soon as the pandemic hit we knew we had to redirect our research towards a COVID-19 vaccine. We believe that our platform can revolutionise vaccine development, and we couldn’t leave it on the shelf while this crisis was unfolding across the world. We’ve been working around the clock, our first vaccine candidates were ready for preclinical trials just weeks after the SARSCoV-2 genome sequence was released, which is unprecedented. Now we need to push these trials forwards and prove our candidates are safe and effective. There’s no time to lose.’
A key advantage of the ADDomer is its incredible stability. Most vaccines have to be kept between 2-8 oC to remain effective, so a ‘cold chain’ must be maintained all the way from manufacture to injection. A power outage anywhere along that journey can break the chain and leave a vaccine unusable, but just one-tenth of the poorest countries’ health care facilities have reliable power supplies. Imophoron’s vaccines can be stored at room temperature as powders, so they don’t rely on the cold chain. This may make their vaccine easier to supply to low- and medium-income countries. Imophoron has designed several vaccine candidates that incorporate specific regions of an important SARSCoV-2 component called the ‘spike protein’. This protein protrudes from the viral surface and binds human cells, allowing the virus to invade. The company’s researchers hope that by only presenting the most important parts of the spike protein, their ADDomers will induce a stronger and safer immune response compared to other vaccine candidates.
Imre Berger, Director of Bristol’s Max Planck Centre for Minimal Biology and cofounder of Imophoron, said: ‘We still have a long road ahead, but COVID-19 research is accelerating at a breathtaking pace. It usually takes a decade to deliver a vaccine, but so many barriers to innovation have fallen recently. Our understanding of this virus is improving every day, and we’ve been able to leverage this knowledge using our expertise in synthetic biology to develop several promising vaccine candidates. Most vaccine candidates don’t make it, but we need as many in the race as possible to be sure that some make it over the line. Science always delivers: we have to keep working and hoping.’ Harry Destecroix, founder of Science Creates and an investor in Imophoron, said: ‘We’re so proud of the incredible effort Fred and the team have put towards fighting this global pandemic. During the peak they were working seven days a week not only accelerating their vaccine platform but also providing key materials for the wider research effort at UNCOVER.’
‘We have so much more to learn about SARSCoV-2, but during this crisis we’re seeing that when we focus and work together, we can expedite that process. It doesn’t hurt to have some good luck too! We’re grateful that we can contribute, and excited to find out what surprises the future holds.’
Understanding the virus
SARS-CoV-2 is a virus: an infectious obligate intracellular parasite. It replicates inside human cells, gaining an advantage at their expense. Viruses rely completely on their hosts – they cannot reproduce on their own – and they infect the body, producing the symptoms of disease.
There’s some debate among microbiologists as to whether viruses are technically alive, or what ‘alive’ even means. Outside of their hosts, viruses exist in a dormant state, waiting until they next encounter a cell to infect. Once they do, viruses use one of the proteins on their surface to specifically recognise and bind to a protein on the cell. The virus then enters the cell and falls apart, releasing its genetic material (DNA or RNA) which encodes all of the information needed to make new viruses and suppress the host’s defences. The host cell’s machinery is hijacked to read this viral ‘code’, and it produces many more viruses, which eventually kill the cell and are released from it.
The virus primarily attacks the lungs, and as the immune system tries to fight off the infection, it causes collateral damage: inflammation. Dead cells caught by friendly fire build up and form pus, which interferes with breathing and produces pneumonia. SARS-CoV-2 can also damage the brain, kidneys, heart, and liver, although we don’t completely understand how this happens.
Learning from the fightback
The fightback against COVID-19 has taught us many things and just keeping up with the breakneck speed of research being conducted is a challenge in itself. As we look towards a ‘new future’ it’s important to reflect on what’s been achieved and acknowledge the people working behind the breakthroughs. The progress that’s been made shows the importance of collective endeavour and how a collaborative approach can accelerate our understanding and drive us all towards a brighter future.
| Antigen | Antibody | |
| What is it? | A molecule that triggers an immune response | A large Y-shaped protein that specifically recognises the structure of an antigen and binds it |
| Where does it come from? | Anything that the immune system recognises can be an antigen: molecules on microbes, pollen, and even your own cells | Antibodies are produced by the white blood cells of the immune system |
About the author:
Henry Stennett is a PhD candidate at the University of Bristol, whose synthetic biology research includes looking for new antibiotics in deep sea sponges.
We may use cookies, web beacons, tracking pixels, and other tracking technologies when you visit our website, please read out privacy policy for more information.
Science Creates St Philips, Albert Road, Bristol, BS2 0XJ
Science Creates Old Market, Midland Road, Bristol, BS2 0NS
Science Creates Ventures LLP “trading as SCVC” (FRN: 933134) is an Appointed Representative of Kin Capital Partners LLP “KCP”, which is authorised and regulated by the Financial Conduct Authority (FRN: 656789).